The U.S. Public Health Service conducted an extensive study of silicosis in the Vermont granite cutting sheds as part of a broad investigation of diseases produced by dust. This 1924 study was the first to measure the relation between the environment and the worker’s physical condition. Federal money became available for the first tuberculosis clinics in 1936. X-ray began to be used for diagnosis. Tuberculosis patients spent months, and often years, in sanatoria, rest cures being the most widely used form of treatment at the time. From 1939 to 1942 there were 110 deaths from tuberculosis in Vermont.The legislature revised and consolidated all the existing health laws into one large Act known as the Omnibus Health Bill, passed in 1951. The Public Health Nursing program expanded to cover the entire state. Before this, only about one-third of Vermont towns had received nursing services.
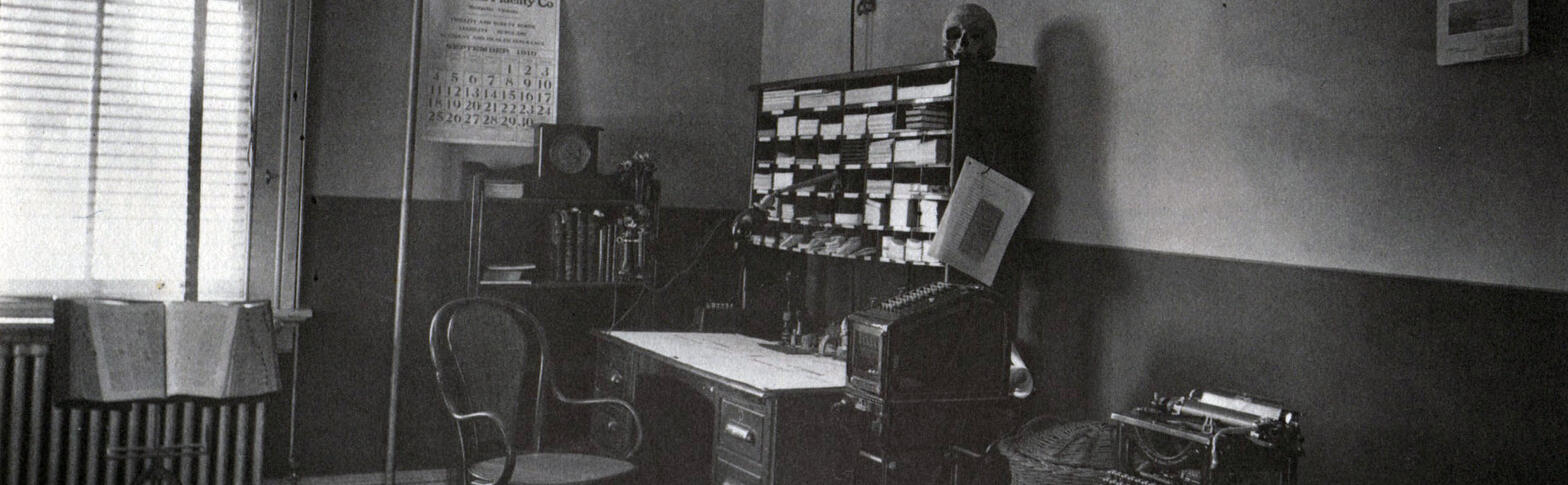
Prior to completion of the new Health Department building on Burlington’s Colchester Avenue in 1953, the Department had occupied an antiquated structure since 1918. A sign on the front of the main portion of the old building read “Oldest Wooden House in Town,1790.”
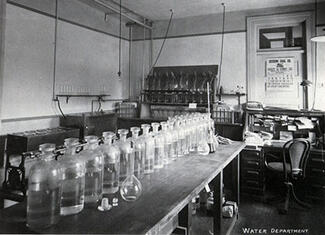
In 1960, it was noted that no deaths from typhoid fever had been reported.
A study was conducted to evaluate lead exposure to people in conjunction with publication of Vermont’s daily newspapers, in which lead type was still widely used, no exposures considered dangerous to health were found.
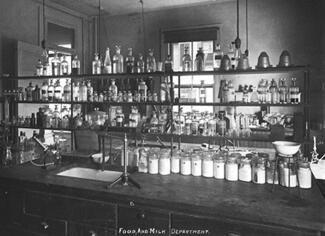
A screening program for kidney, heart, diabetes and gout diseases was implemented by the laboratory in 1963. After a couple of years, the program acquired a van and the clinics became mobile, traveling to industries, schools and other community cites to test children and adults. Recreation trends and changes in traveling habits made their impact on the Health Department in the mid 1960s. The majority of new construction was in the ski areas and around larger municipalities, according to the numbers of food and lodging inspections and licenses issued.
Beginning in 1952, tuberculosis victims were treated with isoniazid, a new drug that signaled the end of the sanatorium era. Patients would be treated and cured with little or no interruption of their lives, and contacts of tuberculosis patients could be treated with the same drug for effective tuberculosis prevention.
In 1952, the City of Burlington became the first Vermont community to provide fluoridated water to its residents. The Centers for Disease Control and Prevention has recognized community water fluoridation as one of the 10 greatest public health achievements of the 20th century.
Pre-operation planning and testing for the Vermont Yankee Nuclear Power plant involved extensive consultation by the Department’s Industrial Hygiene Division (now Occupational and Radiological Health) beginning in 1968. One responsibility was to help set up environmental monitoring stations in the vicinity of the plant site and along the Connecticut river. On November 30, 1972, Vermont Yankee began producing power for public consumption.
Vaccine for rubella (German measles) was introduced in 1969. Vermont’s public health nurses conducted an intensive immunization program, vaccinating 39,000 Vermont school children that year. The legislature passed a law in 1979 which made immunization mandatory for people entering school in Vermont.
The law was designed to protect children from common communicable diseases — rubella, measles, diphtheria, tetanus, pertussis (whooping cough) and polio. Following enactment of the law, there has been a dramatic decrease in the number of rubella and measles cases in Vermont. Diphtheria, tetanus and polio cases had already diminished to a very small number even before 1979.